Chartis, in partnership with the National Rural Hospital Association, conducted a survey and published the results as a paper entitled Vaccine Hesitancy Signals Arrival of Challenging “New Normal” for Rural Hospitals
In this, the latest in a series of “in depth” analyses, I will summarize and comment on the paper.
From the introduction
Our examination of COVID vaccination rates among rural hospital healthcare professionals reveals that despite being an early cohort to have access to COVID vaccines, hesitancy and resistance to vaccination is prevalent. These results are particularly worrisome as they suggest COVID could linger within rural communities for the foreseeable future, stretching hospital resources and further amplifying the risk that many of the most vulnerable populations face regarding population health disparities, racial inequality, and declining access to care.
- While one would expect healthcare providers to accept vaccination as protection against occupational exposure to COVID-19, a significant percentage remain hesitant to get vaccinated
- These individuals add to a similar cohort in their communities, contributing to an at-risk environment as the county seeks to move towards immunity and a return to normal
- Rural communities with pronounced hesitancy and low vaccination rates are examples of potential hot spots to give safe harbor to the virus and serve as potential sources of spread.
In partnership with the National Rural Health Association, the Chartis Center for Rural Health surveyed rural hospital leaders on the topic of COVID vaccination among rural hospital healthcare personnel between March 12, 2021 and April 15, 2021.What we’ve learned through our analysis of the survey data is that:
- COVID vaccine hesitancy and declination are prominent among rural healthcare personnel
- COVID vaccination rates among rural healthcare personnel are lower than influenza vaccination rates
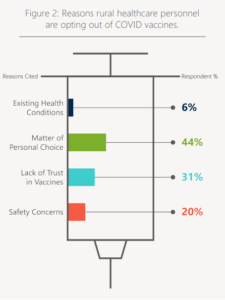
- Vaccine hesitancy and declination is heavily rooted in matters of “personal choice” and “mistrust”
- Rural hospitals continue to actively promote vaccination via education and outreach
An overwhelming majority of respondents — 76 percent — believe that local attitudes regarding COVID vaccines are improving over time. In fact, 43 percent of respondents who answered our request to elaborate via a free-form response on drivers behind changing attitudes cited the impact of knowing others who have had a positive vaccination experience (e.g., no adverse side effects).
This comports with reports from the field, where “early adopters” were regarded as “guinea pigs” by some of their co-workers, and watched for signs of harm. Absent that data, there is a suggestion that those expressing hesitancy are not absolute in their refusal to be vaccinated,
Rural healthcare facilities, as part of their public health mission, have been enlisted in the effort to learn about and enact effective strategies that confront vaccination hesitancy and increase vaccination rates – among their staff and in the communities they serve.
The paper provides information about why rural healthcare facility workers decline – at this point – the opportunity to be vaccinated.
The announcement by the Biden Administration on May 4, 2021, to increase vaccination rates prioritizes the needs of rural communities, and directly addresses the importance of reducing the impact of COVID on rural communities. The coupling of a rural-specific, government-directed vaccination strategy with dedicated local education and outreach efforts on the part of providers may reduce the length of time COVID lingers across rural America and thus alleviate some of the risk and vulnerability felt each day by rural Americans
Chief Operating Officer